What is Epilepsy Surgery?
Epilepsy surgery is a medical procedure designed to treat people with epilepsy whose seizures are resistant to medication. The surgery targets the area of the brain that is responsible for initiating seizures.
Epilepsy is a chronic brain condition in which nerve cells do not signal properly, resulting in recurring seizures. It is also known as a seizure disorder and can affect anyone, irrespective of gender or age.
A seizure is a medical condition in which a sudden and uncontrolled burst of electrical activity happens in the brain. It happens because of a temporary change in the electrical functioning of the brain.
What is Medically Intractable Epilepsy?
Intractable means not easily managed or relieved. Medically intractable epilepsy is also known as drug-resistant epilepsy, in which seizures can’t be completely controlled by medication.
What is Medically Refractory Epilepsy?
Medically refractory epilepsy is a condition that involves epilepsy that is resistant or unresponsive to medical treatment. In this case, you experience seizures even after using various medications and other treatment options.

Which Disease Can Be Treated with Epilepsy Surgery?
Following are the types of epilepsy that can be treated through surgery:
- Mesial temporal lobe epilepsy
- Neocortical epilepsy
- Focal epilepsy
- Hemispheric epilepsy
- Other severe and drug-resistant epilepsy
Causes and Symptoms of Epilepsy
There is no identifiable cause for epilepsy. However, there are certain risk factors, such as genetic influence, head trauma, injuries before birth, and developmental disorders.
Signs and symptoms of epilepsy depend on their type. Some of the symptoms include:
- Seizures
- Unusual sensations, emotions, or visual disturbances
- Temporary confusion
- Loss of consciousness
- Uncontrolled movements
- Stiff muscles

What are the indications for epilepsy surgery?
- Experiencing frequent seizures
- Failure of other treatments
- Side effects of anti-seizure medications
- Focal epilepsy
- Medication intolerance
What Are the Different Options for epilepsy surgery?
Epilepsy surgery is a brain surgery to reduce the frequency and severity of the seizures you’re experiencing. Surgical options for epilepsy management are considered when anti-seizure medications are not working well in one’s condition and if the seizures are severe and debilitating.
There are many types of surgical procedures available to manage seizures, including:
01. Surgical Resection
Resection surgery is the most common type of epilepsy surgery. In this surgery, neurosurgeons remove the specific area of the brain causing seizures to remove or treat epilepsy. There are several types of resection, such as:
- Lesionectomy
It is a common surgical procedure to remove a lesion, known as an abnormally functioning area in the brain. This procedure is performed under general anaesthesia and removes lesions such as tumours, cavernous haemangiomas, and arteriovenous malformations that can cause seizures. Most people find complete seizure control after this procedure.

- Lobectomy
Lobectomy is another operation that is done to manage and treat people who are dealing with epilepsy. This surgery is done on a person experiencing seizures from a well-defined area in the brain. During this surgery, the neurosurgeon removes the lobe where seizures begin.

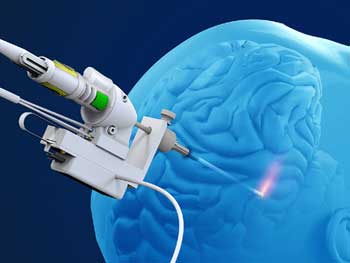
02. Laser interstitial thermal therapy (LITT)
It is a minimally invasive surgical option that is used to treat medical conditions such as epilepsy. As the name suggests, it uses laser technology to target and destroy the abnormal brain tissues in the brain that lead to seizures.
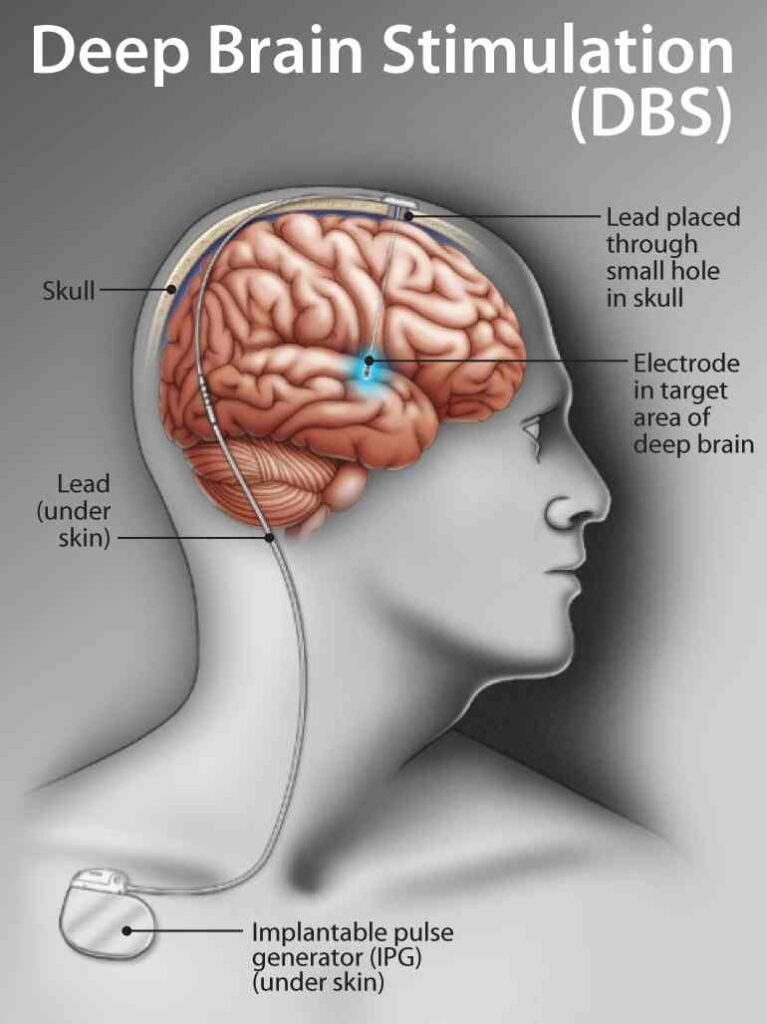
03. Deep Brain Stimulation (DBS)
It is a medical technique that includes the implantation of electrodes in specific brain areas for the treatment of epilepsy. It is one of the types of neuromodulation therapy that is used together with the medication. This surgery includes the implantation of an electrode in the brain and the placement of a stimulator device under the skin in your chest. After this, the stimulator device gives signals to the electrode to receive signals from the nerve cells that trigger the seizures.
04. Hemispherectomy
‘Hemi’ means half, which represents the cerebral (brain) hemisphere, i.e., half of the brain. This surgical method is used to treat epilepsy when seizures are not controlled with medication. This procedure includes the removal of the entire cerebral hemisphere to stop the seizures. Hemispherectomy is generally done in children and occasionally in adults.
05. Corpus Callosotomy
Corpus callosotomy is a procedure that severs the corpus callosum, the bundle of nerve fibres connecting the brain’s two hemispheres. This procedure is typically performed in cases of severe epilepsy when seizures cannot be controlled by other means. It helps prevent seizures from spreading across the brain but does not eliminate them.
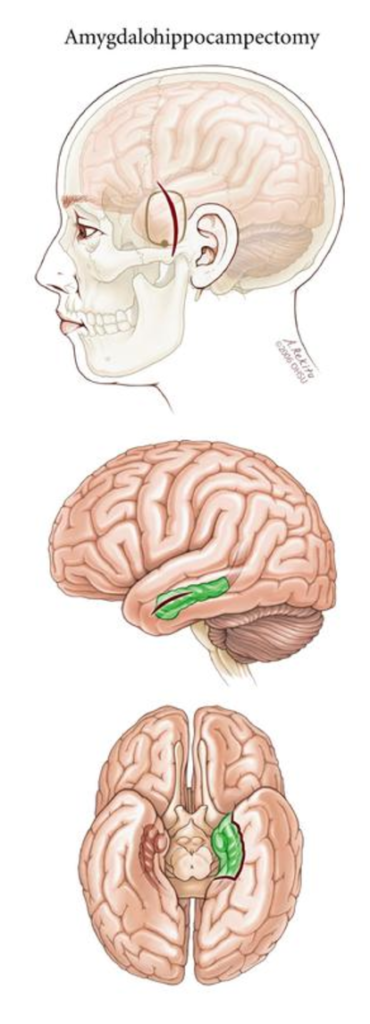
06. Amygdalohypocampectomy
It is a surgical intervention used to treat all drug-resistant epilepsy (DRE) that usually originates in the hippocampus and the temporal lobe. This surgery includes the partial resection and removal of a specific part of the brain, which is the amygdala and the hippocampus. It is considered a safe and effective procedure for managing temporal lobe epilepsy.
CONCLUSION
Epilepsy is a common neurological disorder that can lead to several seizures. If medications haven’t worked to control the seizures, doctors may opt for surgical options to treat and manage the epilepsy.
There are various surgical treatment options available to treat this chronic brain condition. Some of the options have been discussed in this blog, like lobectomy, hemispherectomy, and deep brain stimulation (DBS).
However, these surgical options depend on the severity and location of the seizures in the brain. It is important to consult your neurosurgeon before going through any examinations or treatments.
A brain cyst is a fluid-filled sac or lesion that forms within the brain tissue or in its surrounding membranes. The cyst is mostly benign, which means it does not lead to any cancer but can affect the daily routine of an individual in ways such as headaches, vision problems, nausea and vomiting, seizures, and many others.
What Is an Intraventricular Brain Cyst?
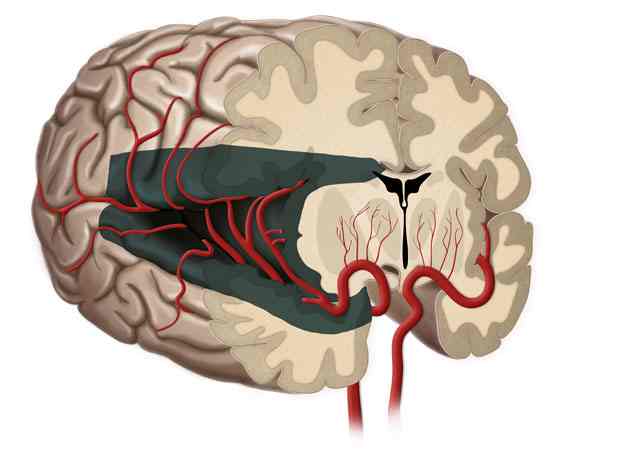
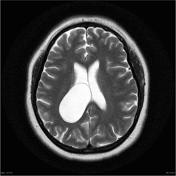
The intraventricular cyst is a condition in which the development of cysts occurs within the brain ventricles.
Ventricles are the cavities in the brain that are responsible for the production and storage of cerebrospinal fluid. CSF is a watery fluid that surrounds your brain and spinal cord and also helps provide cushioning and protection from any trauma. It also removes waste and provides nutrients to your brain.
When a cyst develops in any of the ventricles, it can disrupt the cerebrospinal fluid’s normal flow and functioning, leading to various potential complications.
Colloid Cyst:
A colloid cyst is a type of brain cyst that typically develops in the third ventricle of the brain. The third ventricle is one of the four interconnected cavities within the brain responsible for cerebrospinal fluid (CSF) circulation. Colloid cysts are filled with a thick, gel-like substance called colloid material. While these cysts are generally considered benign, they can cause problems by obstructing the normal flow of cerebrospinal fluid.
Causes and Symptoms of an Intraventricular Brain Cyst
The causes of intraventricular brain cyst are still unknown and can vary from person to person. It is believed that some cysts are congenital, i.e., present at birth due to some fetal abnormalities, and others may be acquired later in life, like head injuries, inflammation within the brain, and infections.
Signs and symptoms of an intraventricular brain cyst include persistent headaches that worsen over time, blurred or double vision, changes in mood and behaviour, and difficult concentration and coordination issues.
Surgical Options for Intraventricular Cysts
Treatment options for intraventricular cysts are considered when the cyst in the ventricles may press the brain tissue and cause symptoms or when it becomes enlarged. Treatment is also recommended when the cyst blocks the normal flow of cerebrospinal fluid.
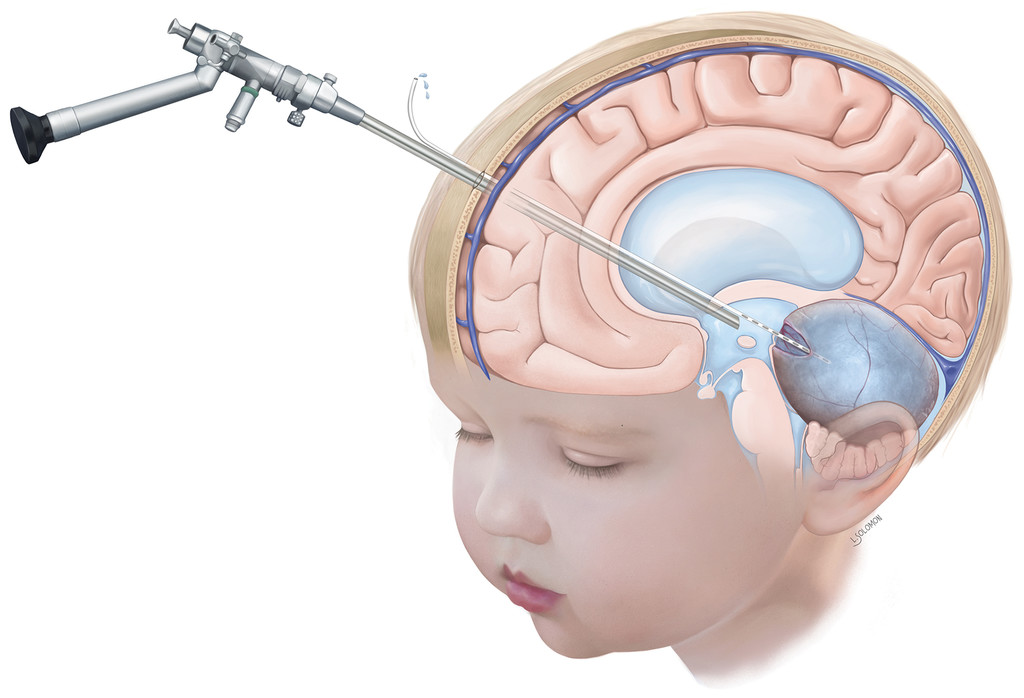
Neuroendoscopic options to treat your intraventricular cyst:
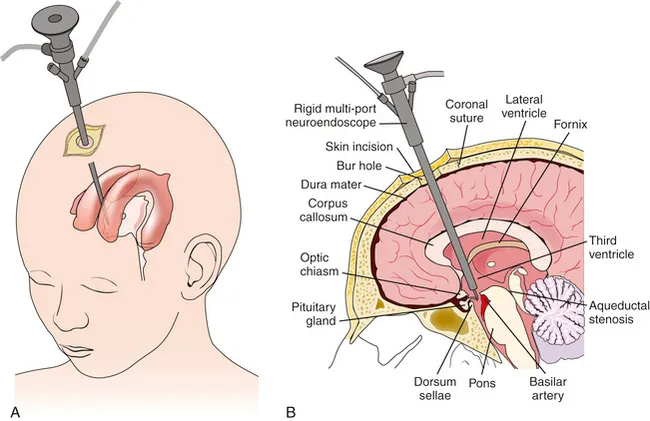
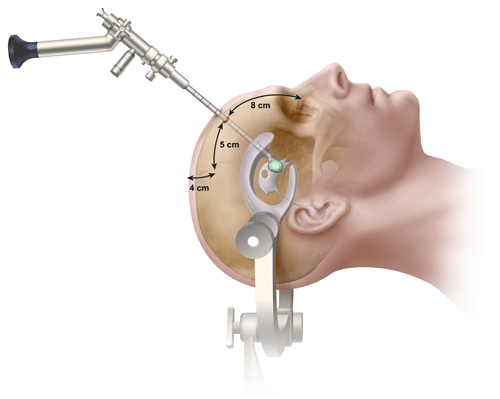
Neuroendoscopy is a minimally invasive surgical procedure that is used to treat intraventricular cysts that develop in the brain’s ventricles. Under neuroendoscopy, several treatments are classified based on the type, characteristics, and location of the cyst. It also depends on the patient’s overall health, and below are some of the surgical options that use neuroendoscopy to treat intraventricular cysts.
- Cyst fenestration
One of the best and most effective treatments for intraventricular cysts is endoscopic cyst fenestration. It is a minimally invasive procedure that includes creating an opening, also known as fenestration, in the cyst while using an endoscope.
During this surgical procedure, the surgeon inserts the endoscope into the ventricles to help doctors look out the cyst and carefully create an opening in the cyst. Creating the opening in the cyst, allows the cyst’s contents (cerebrospinal fluid) to drain into the surrounding ventricle or brain tissue.
2. Cyst resection
There are different types of intraventricular cysts, and so there are treatments. It is necessary to completely remove the solid and thick-walled intraventricular cyst.

For this, surgeons choose the neuroendoscopic cyst resection method. This surgical method involves using an endoscope to carefully visualise the cyst and dissect it from the surrounding tissue.
After removing the cyst, the patient will not experience any symptoms or complications associated with the cyst.
3. Endoscopic Third Ventriculostomy (ETV)
This procedure is performed when the intraventricular cyst interferes with the flow of the cerebrospinal fluid within the ventricles. During ETV, doctors, by using an endoscope, create an opening in the floor of the third ventricle that helps allow the fluid to bypass the cyst and resume its normal functioning.
Neuroendoscopy for intraventricular cysts offers several benefits such as less invasive, shorter recovery period, and hospital stays as compared to traditional surgery.
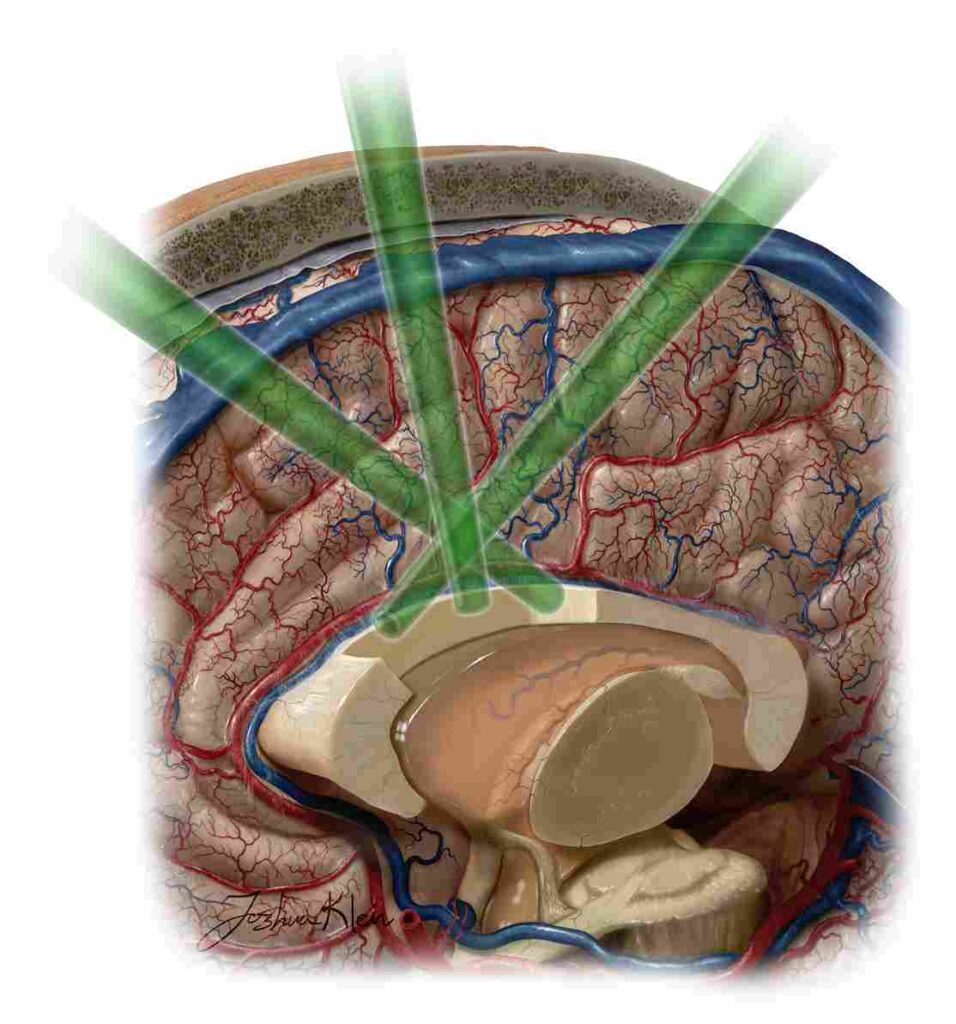
4. Endoscopic Excision of Colloid Cysts
One of the most advanced and minimally invasive methods for excising colloid cysts is through neuroendoscopy. Here’s how the procedure typically works:
- The patient is prepared for surgery, which may involve general anaesthesia or sedation.
- Endoscope Insertion: A neurosurgeon makes a small incision in the scalp and inserts a thin, flexible tube called an endoscope through a small burr hole in the skull. The endoscope has a light source and a camera that allows the surgeon to see inside the brain.
- Cyst Visualization: The surgeon navigates the endoscope to reach the location of the colloid cyst within the third ventricle. The camera provides a clear view of the cyst and surrounding structures.
- Cyst Resection: Using specialized instruments passed through the endoscope or by using laser technology, the surgeon carefully removes the colloid cyst and any obstructive material. The goal is to completely excise the cyst while minimizing damage to surrounding brain tissue.
- Closure: Once the cyst has been excised, the surgeon closes the incision, often with sutures or staples.
CONCLUSION
An intraventricular cyst is usually a benign cyst, but it can also lead to some discomfort and complications in individuals. To help alleviate the discomfort of people dealing with this problem, surgeons use specific approaches and techniques involving neuroendoscopy. It is important to consult a skilled neurosurgeon with extensive experience and specialising in neuroendoscopy.





